Summary
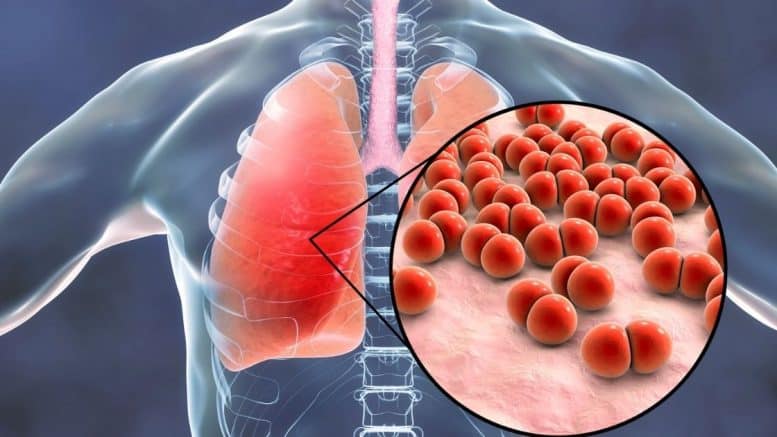
Contents showCommunity-acquired Pneumonia is a common infection of the lower respiratory tract, most commonly produced by bacterial pathogens.
The pathophysiology of community-acquired pneumonia consists of the interplay of host’s and pathogen’s factors, producing an acute inflammatory response in the lung tissue.
Diagnostic strategies include clinical history, physical examination, laboratory studies, imaging, and microbiological studies in selected cases. Antibiotic therapy is the mainstay of treatment, which usually starts with empirical antibiotic regimens.
Introduction to Community-Acquired Pneumonia
Pneumonia is one of the most common and severe causes of demise in adult patients worldwide. It is also a significant cause of morbidity across the world. The prompt recognition, risk stratification, and treatment of this condition reduce morbidity and mortality in those affected.
This article aims at explaining the most common causes and clinical presentations of community-acquired pneumonia (CAP) among adults in the outpatient setting and focuses on the appropriate risk stratification and assessment of patients with bacterial Community-Acquired Pneumonia. Viral pneumonia, ventilation-associated pneumonia, and hospital-acquired pneumonia will be treated in separate articles.
Definition of Community-Acquired Pneumonia
CAP is a clinical syndrome in which an individual presents signs and symptoms of lower respiratory tract infection, evidence of new pulmonary infiltrates, and inflammatory response acquired outside the hospital.
Classification of Community-Acquired Pneumonia
Community-Acquired Pneumonia is classified according to patients’ clinical presentations in: (1)
- Typical CAP: classic symptoms of fever, cough productive of mucopurulent sputum, dyspnea, pleuritic chest pain, and condensation syndrome on physical exam.
- Atypical CAP: flu-like illness consisting of dry cough, malaise, myalgia, low-grade or no fever, unremarkable physical exam.
According to the location: (2)
- Lobar pneumonia: pulmonary condensation affecting one pulmonary lobe.
- Interstitial pneumonia: infiltration of the interstitium, sometimes affecting alveolar spaces.
- Bronchopneumonia is a syndrome involving multiple patchy infiltrates affecting the bronchi and alveolar spaces. It may affect multiple lobes.
Epidemiology of Community-Acquired Pneumonia
Pneumonia is responsible for high morbidity and increased mortality risk in hospitalized individuals requiring intensive care unit (ICU) admission. (3)
The annual incidence in the USA for young adults is estimated at 24.8-106 cases/10,000 people/year. (4)
Incidence increases with age, as the process of immunosenescence and increased rate of comorbidities overcomes, reaching up to 164.3/10,000 people/year in those older than 80. (5)
Etiology and relative frequencies (4)
Outpatients
| Streptococcus pneumoniae | 35 % |
| Atypical bacteria | 36 % |
| Mycoplasma pneumoniae | 17 % |
| Legionella pneumophila | 6 % |
| Chlamydophila pneumoniae | 6 % |
| Coxiella burnetii | 7 % |
| Respiratory viruses | 9 % |
| Haemophilus influenzae | 5 % |
| Polymicrobial etiology | 9 % |
| Pseudomonas aeruginosa | 1 % |
| GNEB | 1 % |
| Staphylococcus aureus | 1 % |
Approach to the Patient:
Key points:
- Approach every patient presenting to the acute setting according to the ABCDE approach.
- Diagnose pneumonia and possible complications.
- Risk stratification.
- Install antibiotic treatment as soon as possible.
Patients may be concerned with specific or unspecific symptoms on the first encounter.
The most common symptoms are those of lower respiratory infection, such as chest pain, cough with sputum production, fever, malaise, and dyspnea.
In several other cases, symptoms may be unspecific and challenging to address, especially in elderly patients, such as asthenia, hyporexia, decreased functionality, irritability, altered level of consciousness, hypothermia, and dehydration.
Note: an elderly patient presenting with unspecific symptoms such as altered mental status, difficulty feeding or drinking, irritability, or somnolence, may have an infection!
Have full documentation of vital signs and a complete medical history, including allergies, chronic diseases, travel, contact with sick people, risk of zoonoses, job exposure, and review of systems.
Physical examination consists of a complete evaluation of the patient, especially those with comorbidities, as infections commonly cause exacerbations or decompensation of chronic diseases.
The respiratory system examination can yield:
- Inspection: decreased breathing movement, altered ventilatory mechanics, tachypnea, use of accessory muscles, cyanosis.
- Palpation: unilateral or bilateral decrease in a pulmonary excursion. Augmented vocal vibrations if underlying condensation.
- Percussion: dullness.
- Auscultation: crackles if condensation along with bronchophony or egophony. Pleural sounds if pleural effusion is present.
Risk factors:
Risk factors associated with CAP: (6)
- Age
- Male gender
- COPD
- Chronic alcohol use
- Smoking
- Upper respiratory tract infections
- Congestive Heart Failure
- Immunodeficiency
- Cerebrovascular disease
- Liver Disease
- Diabetes mellitus
- Chronic Renal Failure
- Malignancy
- Corticosteroid therapy
Risk factors for Pseudomonal infection: (7)
- Immunocompromised patients, especially those with cystic fibrosis or acquired immune deficiency syndrome.
- Bronchiectasis.
- Neutropenia.
- Burns.
- Oncologic disease.
- Organ transplant.
- Uncontrolled diabetes mellitus.
- ICU admission.
- Invasive devices.
Risk factors for Methicillin Resistant Staphylococcus Aureus (MRSA) infection: (8)
- Prolonged hospitalization.
- ICU admission.
- Recent antibiotic use.
- History of MRSA colonization.
- Invasive procedures.
- Immunocompromise
- Admission to nursing homes.
- Open wounds.
- Hemodialysis
- Discharge with long-term central venous access.
- Indwelling urinary catheter.
Pathophysiology and Presentation
There are three recognized routes of transmission of respiratory pathogens: inhalation, aspiration, and hematogenous spread.
Pathogens transmitted via inhalation are transported through microdroplets, and depending on several hosts and microorganism factors, respiratory pathogens may stay in suspension in the lower respiratory tract, accounting for the first phase of infection. (4)
Decreased mucociliary clearance, impaired secretion of mucosal immunoglobulins, and increased reactive oxidative damage permit the interaction of pathogens to the respiratory mucosa. Infection results from reproducing pathogens in the respiratory tract and their interaction with the immune system. (4)
In the case of streptococcus pneumoniae, a series of virulence factors play a role in infection initiation. The essential one is its polysaccharide capsule, which impedes opsonization by alveolar macrophages. (9)
At that time, if bacteria outnumber macrophages, a robust pro-inflammatory reaction ensues with the secretion of IL-1, IL-6, and TNF alfa. Neutrophils are recruited by chemotaxis, producing an alveolar inflammatory infiltrate. Due to the pro-inflammatory state, the patient experience unspecific symptoms like fever, malaise, and asthenia. Alveolar infiltrates stimulate cough mechanisms with mucopurulent sputum production, and if inflammation involves the pleura, the host experiences pleural pain. (9)
Pseudomonas Aeruginosa infection usually ensues in immunocompromised patients or those with wide-spectrum antibiotic usage and should be suspected in any patient with sepsis or systemic infection. Virulence factors include intrinsic resistance to antibiotics, efflux pumps, and enzymatic cleavage of antibiotic molecules. (7)
MRSA is a pathogen of concern, usually encountered in patients with risk factors, although its prevalence among CAP patients is increasing. Originally described as a complication of influenza pneumonia, there have been cases of isolated MRSA infection in healthy individuals. (8)
The Mec-A gen, transmitted by bacteriophages, is responsible for the transcription of beta-lactamase enzymes, which account for its known antibiotic resistance pattern. Patients are at high risk of rapidly progressive infection associated with fever, bloody sputum, hypotension, and the development of septic shock. (8)
Diagnosis
Clinical diagnosis alone is not always sufficient for the diagnosis of CAP. Further diagnostic tools are relevant to address the need to install antibiotic treatment if necessary.
Lab studies and relevant findings include:
- Complete blood count: leukocytosis, leukopenia, anemia, thrombocytopenia.
- CRP, ESR: increased CPR is associated with bacterial pneumonia with low sensitivity.
- Basic metabolic panel: address normal metabolic function.
- Liver enzymes: liver function, part of the assessment for sepsis.
- ABG: relevant in patients in whom hypoxia is suspected, or SpO2 ≤94% at room air. Relevant to address ventilatory function and oxygenation.
- Procalcitonin: aids with the decision to install antibiotic treatment. Increased procalcitonin is associated with a bacterial infection. Normal levels can be due to viral pneumonia, confined infection such as abscess, or immunosuppression.
Radiological studies address the suspicion of a pulmonary infiltrate.
A chest X-ray is the first choice of diagnostic measurement. Pulmonary infiltrate may vary according to the underlying disease and could be lobar infiltrate or interstitial in the case of atypical pneumonia. (10)
In some cases, a thoracic CT scan without contrast could help when there are unspecific findings in the chest x-ray but still high clinical suspicion of pneumonia. It is also helpful to address complications of pneumonia and associated comorbidities. (11)
Microbiological Studies in Community-Acquired Pneumonia
Sputum analysis or blood cultures are not routinely recommended for ambulatory patients with no risk factors for MRSA of Pseudomonal infection. The IDSA/ATS 2019 guidelines for the diagnosis and management of pneumonia states clear scenarios where these tests are recommended: (12)
- In severe CAP (especially if they are intubated).
- When an empirical treatment for MRSA or Pseudomonas aeruginosa will be performed.
- When the patient has been infected with MRSA and/or P. Aeruginosa (especially those with prior respiratory tract infection).
- In patients who were hospitalized and received parenteral antibiotics during the last 90 days.
Legionella tests, as well as respiratory virus detection, are recommended in patients on whom an epidemiological context is relevant (close contact, travels). (12)
There is still a low level of evidence to address the microbiological analysis of patients with CAP. In three studies evaluating mortality, there was no statistical difference between groups, and guidelines point to the need for more research on this aspect. (13, 14, 15)
Risk-stratification
CURB-65 and PSI/PORT scores are tools designed to assess 30-day mortality from the time of diagnosis. These two are used to aid in the decision of hospitalization. Clinical guidelines recommend their use along with clinical judgment. (12)
One should use them as an adjunct to clinical judgment and should never replace the latter. Certain situations not evaluated with these tools may confer the need for hospitalization, such as improper oral intake, unavailable relative support, or decreased functionality.
CURB-65 score: (16)
- Confusion (disorientation, impaired consciousness)
- Serum Urea > 7 mmol/L (20 mg/dL)
- Respiratory rate ≥ 30/min
- Blood pressure: systolic BP ≤ 90 mm Hg or diastolic BP ≤ 60 mm Hg
- Age ≥ 65 years
A score of 2 points correlates with the need for hospital admission.
The 30-day mortality rate correlation with scores is as follows:
- 0 points, 0%.
- 1 point, 1.1%.
- 2 points, 7.6%.
- 3 points, 21%.
- 4 points, 41.9%.
- 5 points, 60%.
PSI/PORT score: (17)
This score consists of 20 items created by Dr. Fine in 1997 and has been validated to aim in the decision of inpatient vs. outpatient treatment. Validation processes have been performed, and it is believed that the score could underestimate severe pneumonia in younger patients. (12)
IDSA/ATS criteria: (12)
This tool is to solely address the severity of CAP and to help clinicians assess the level of care that patients may need.
One positive major criterium or three minor criteria reflect the need for ICU treatment and monitoring.
Major criteria
- Septic shock with the need for vasopressors.
- Respiratory failure requiring mechanical ventilation.
Minor criteria
- Respiratory rate ≥30 breaths/min.
- PaO2/FIO2 ratio ≤250.
- Multilobar infiltrates.
- Confusion/disorientation.
- Uremia (blood urea nitrogen level ≥20 mg/dl)
- Leukopenia (white blood cell count ≤4,000 cells/ml).
- Thrombocytopenia (platelet count ≤100,000/ml).
- Hypothermia (core temperature ≤36.8ºC)
- Hypotension requiring aggressive fluid resuscitation.
Management of Community-Acquired Pneumonia
The mainstay of treatment is to approach the patient by the ABCDE rules.
- Airway management.
- Oxygenation and mechanical ventilation if indicated.
- Fluid infusion if hypotension or septic shock.
- Assess neurological status.
Once resuscitation measurements have been established when necessary, antibiotic treatment is the following crucial point to address since it has been shown that the earlier antibiotics are started, the better the prognosis. (6)
Empirical Antibiotic Treatment for Community-Acquired Pneumonia(12)
| Outpatient treatment, no comorbidities. | Amoxicillin 1000mg PO, 3 times daily. OR Macrolide: azithromycin 500mg PO, initial dose, then 250mg daily or Clarithromycin 500mg PO twice a day, or Clarithromycin 1000mg PO extended release daily. OR Doxicyclin 100mg PO twice a day. |
| Outpatient treatment with comorbidities such as chronic heart, lung, renal, or liver disease, diabetes mellitus, alcoholism, oncologic disease, or asplenia. | Combination therapy: Amoxicillin/clavulanic acid 500mg/125mg three times daily, or amoxicillin/clavulanic acid 875mg/125mg twice a day, or amoxicillin/clavulanic acid 2000mg/125mg twice a day, or cefpodoxime 200mg twice a day, or cefuroxime 500mg twice a day, AND Macrolide or doxicyclin, same doses as mentioned for previous groups of patients. OR Monotherapy: Levofloxacin 750mg daily, or moxifloxacin 400mg daily, or gemifloxacin 320mg daily. |
| Initial inpatient treatment for patients with no risk factors for MRSA or P. Aeuriginosa. | Combination therapy: Ampicillin+Sulbactam 1.5/3mg every 6 hours, or cefotaxime 1-2g every 8hs, or ceftriaxone 1-2g daily, or ceftaroline 600mg every 12hs, AND Macrolide: azithromycin 500mg daily or clarithromycin 500mg twice a day, or Monotherapy Levofloxacin 750mg daily, or moxifloxacin 400mg daily. |
| Initial inpatient treatment for patients with severe CAP and no risk factors for MRSA or P. Aeuriginosa. | Betalactam and a macrolide (same drugs and regimens as previous section). OR Betalactam and a respiratory fluoroquinolone (same drugs and regimens as previous section). |
| Initial inpatient treatment for patients with CAP and locally validated risk factors for MRSA. | Vancomycin 15mg/kg every 12hs (adjust according to vacomycinemia). OR Linezolid 600mg every 12 hs. |
| Initial inpatient treatment for patients with CAP and locally validated risk factors for P. Aeruginosa. | Piperacillin+tazobactam 4.5g every 6hs or, Cefepime 2g every 8hs or, Ceftazidime 2g every 8hs or, Aztreonam 2g every 8hs or, Meropenem 1g every 8hs or, Imipenem 500mg every 6hs. |
Duration of treatment for non-severe CAP may be 5-7 days, and patients should be assessed 48-72 hs after initiation of treatment to address response to treatment. (12, 18, 19).
Disclosures:
The author does not report any conflict of interest.
Disclaimer:
This information is for educational purposes and is not intended to treat disease or supplant medical professional judgment. Physicians should follow local policy regarding the diagnosis and management of medical conditions.
See Also
Dyspnea Due to Respiratory Causes
Heart Failure With Preserved Ejection Fraction
Acute Upper Respiratory Infections
References:
- Bedi RS. Community acquired pneumonia-Typical or atypical?. Lung India. 2006 Jul 1;23(3):130-1.
- Jain V, Vashisht R, Yilmaz G, Bhardwaj A. Pneumonia pathology. [cited: 9/21/2022]. Availabre from: https://europepmc.org/article/nbk/nbk526116
- Cavallazzi R, Furmanek S, Arnold FW, Beavin LA, Wunderink RG, Niederman MS, Ramirez JA. The burden of community-acquired pneumonia requiring admission to ICU in the United States. Chest. 2020 Sep 1;158(3):1008-16.
- Cillóniz C, Cardozo C, García-Vidal C. Epidemiology, pathophysiology, and microbiology of community-acquired pneumonia. Ann Res Hosp. 2018;2(1):1-1.
- Ferreira-Coimbra J, Sarda C, Rello J. Burden of community-acquired pneumonia and unmet clinical needs. Advances in therapy. 2020 Apr;37(4):1302-18.
- Ticona JH, Zaccone VM, McFarlane IM. Community-acquired pneumonia: A focused review. Am J Med Case Rep. 2021 Nov;9(1):45-52.
- Wilson MG, Pandey S. Pseudomonas Aeruginosa. InStatPearls [Internet] 2022 May 1. StatPearls Publishing. [cited: 9/21/2022]. Availabre from: https://www.ncbi.nlm.nih.gov/books/NBK557831/
- Siddiqui AH, Koirala J. Methicillin resistant Staphylococcus aureus. InStatPearls [internet] 2021 Jul 19. StatPearls Publishing. [cited: 9/21/2022]. Availabre from: https://www.ncbi.nlm.nih.gov/books/NBK482221/
- Wootton DG, Aston S, Gordon S. The pathophysiology of pneumococcal pneumonia. Community-Acquired Pneumonia: European Respiratory Monograph. 2014 Mar 1;63:1879.
- Parveen N, Sathik MM. Detection of pneumonia in chest X-ray images. Journal of X-ray Science and Technology. 2011 Jan 1;19(4):423-8.
- Claessens YE, Debray MP, Tubach F, Brun AL, Rammaert B, Hausfater P, Naccache JM, Ray P, Choquet C, Carette MF, Mayaud C. Early chest computed tomography scan to assist diagnosis and guide treatment decision for suspected community-acquired pneumonia. American journal of respiratory and critical care medicine. 2015 Oct 15;192(8):974-82.
- Metlay JP, Waterer GW, Long AC, Anzueto A, Brozek J, Crothers K, Cooley LA, Dean NC, Fine MJ, Flanders SA, Griffin MR. Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the American Thoracic Society and Infectious Diseases Society of America. American journal of respiratory and critical care medicine. 2019 Oct 1;200(7):e45-67.
- Waterer GW, Jennings SG, Wunderink RG. The impact of blood cultures on antibiotic therapy in pneumococcal pneumonia. Chest. 1999 Nov 1;116(5):1278-81.
- Benenson RS, Kepner AM, Pyle II DN, Cavanaugh S. Selective use of blood cultures in emergency department pneumonia patients. The Journal of emergency medicine. 2007 Jul 1;33(1):1-8.
- Lidman C, Burman LG, Lagergren Å, Örtqvist Å. Limited value of routine microbiological diagnostics in patients hospitalized for community-acquired pneumonia. Scandinavian journal of infectious diseases. 2002 Jan 1;34(12):873-9.
- Capelastegui A, Espana PP, Quintana JM, Areitio I, Gorordo I, Egurrola M, Bilbao A. Validation of a predictive rule for the management of community-acquired pneumonia. European Respiratory Journal. 2006 Jan 1;27(1):151-7.
- Fine MJ, Auble TE, Yealy DM, Hanusa BH, Weissfeld LA, Singer DE, Coley CM, Marrie TJ, Kapoor WN. A prediction rule to identify low-risk patients with community-acquired pneumonia. New England journal of medicine. 1997 Jan 23;336(4):243-50.
- Foolad F, Huang AM, Nguyen CT, Colyer L, Lim M, Grieger J, Li J, Revolinski S, Mack M, Gandhi T, Wainaina JN. A multicentre stewardship initiative to decrease excessive duration of antibiotic therapy for the treatment of community-acquired pneumonia. Journal of Antimicrobial Chemotherapy. 2018 May 1;73(5):1402-7.
- Tansarli GS, Mylonakis E. Systematic review and meta-analysis of the efficacy of short-course antibiotic treatments for community-acquired pneumonia in adults. Antimicrobial agents and chemotherapy. 2018 Sep 1;62(9):e00635-18.
Follow us