Summary
Contents showHip fractures are a common medical problem in elderly patients, usually produced by falls, and with an upward trend in the last decades. Hip fractures might significantly impair the patient’s quality of life and pose a burden to the patient’s family.
Diagnosis of hip fractures results from a clinical and radiographic assessment. Initial medical therapy and appropriate surgical planning are necessary to improve outcomes and prevent complications and disability.
Introduction to Initial Management of Hip Fractures in Adults
Hip fractures are a frequent injury in the geriatric population. Around 90% occur in people over 65 years old [1]. In the last decade, there were an estimated 250,000 cases per year in the United States, with an increasing trend because of the aging population [2].
The etiology underlying these injuries in older adults is low-energy falls from one’s height; in younger patients, they usually result from high-energy impacts, such as vehicle accidents.
Society’s burden remains high despite available options for hip fracture prevention. An 8-36% excess in mortality within 1 year of injury [3], problems for patient’s relatives, and high healthcare system costs are some associated problems [4].
The purpose of this article is to explore the different types of fractures in the hip joint, emphasizing femoral neck and trochanteric fractures, how to perform an uneventful diagnostic, the initial clinical management, and briefly outline the different surgical treatment options.
Definition of Hip Fractures
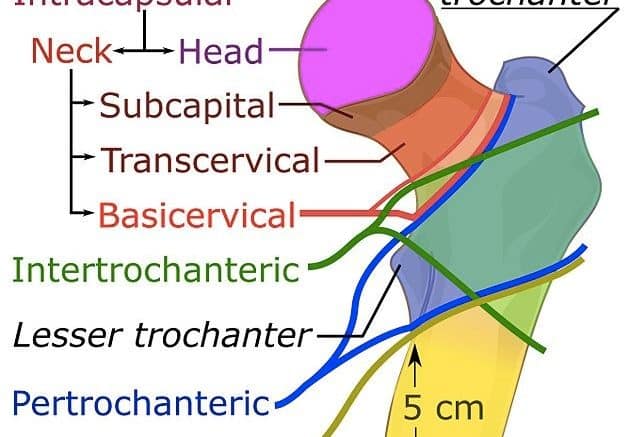
The hip joint, or coxofemoral joint, is a ball and socket joint, the articulation between the proximal epiphysis of the femur (the femoral head) and the acetabulum in the pelvis. However, when we talk about Hip Fractures, we refer to fractures involving any part of this proximal epiphysis or metaphysis of the femur, which includes the femoral head, the femoral neck, and the trochanters. Figure 1.
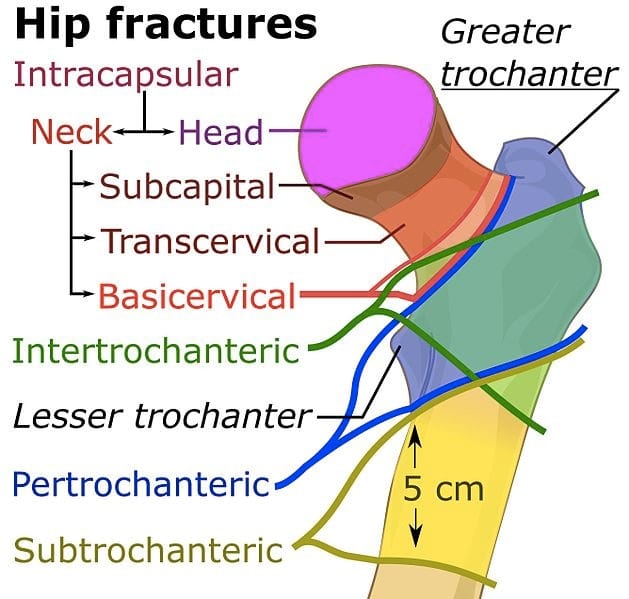
Figure 1. Zones where a hip fracture can occur. Mikael Häggström, using image by Mariana Ruiz Villarreal (LadyofHats, CC0, via Wikimedia Commons)
Case example: A 75-year-old female presents to the emergency department after a mechanical fall in the grocery store parking lot. Her leg is shortened and externally rotated. She can not bear weight nor sit without pain. Radiographs demonstrate a displaced femoral neck fracture. Upon further questioning, she states she is active, plays golf twice a week, and does not use assistive devices. She denies antecedent hip pain. Radiographs and CT scans are obtained, shown in Figure 2. The patient is admitted to the hospital and will be taken tomorrow to the OR to perform a Total Hip Arthroplasty.
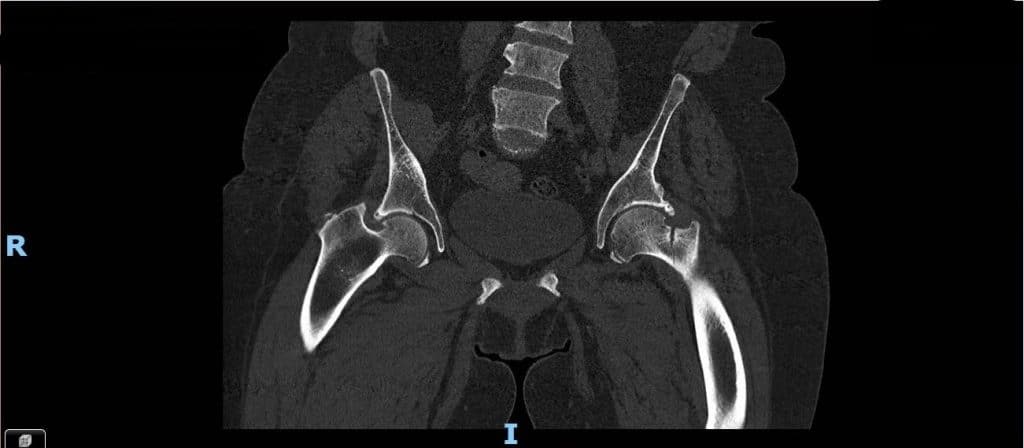
Figure 2. CT scan of a left hip showing a complete nondisplaced transcervical femoral
Epidemiology of Hip Fractures
Approximately 1.6 million hip fractures occur worldwide yearly, by 2050, this number could reach between 4.5 million and 6.3 million. Countries with the higher incidence are the United States and Scandinavian countries [5].
Age is the leading risk factor for hip fractures; the incidence of hip fractures increases exponentially with age: 52% of hip fractures occur after the age of 80 years and 90% after the age of 65 years [6].
Femoral neck and Pertrochanteric fractures are the most common among all hip fractures, and they occur mainly in the elderly with a similar overall incidence. Women are more prone to suffer a hip fracture (some studies show more than double the incidence), and Caucasians are at higher risk. In caucasian women, the lifetime risk of hip fracture is 1 in 6. A 50-year-old woman has a 2.8% risk of death related to hip fracture during her remaining lifetime. Moreover, up to 20% of patients die in the first year following hip fractures, mainly due to pre-existing medical conditions. Less than half of those who survive the hip fracture regain their previous level of function [2].
On the other hand, femoral head fractures are rare traumatic injuries that are usually associated with hip dislocations and high mortality and disability rate, occurring primarily at younger ages and caused by high-energy trauma.
Etiology of Hip Fractures
The decline in bone mineral density and the increase in the frequency of falls in elderly people are mainly responsible for this high incidence. Only 1% of falls lead to a hip fracture, but 90% of these fractures are related to a fall from a standing height or less.
In contrast, young people are prone to suffer high-energy accidents resulting in hip fractures and dislocations.
Classification of Hip Fractures
Hip fractures can be divided into Intracapsular or medial (within the limits of the capsule insertion), which are femoral head and femoral neck fractures, or Extracapsular or lateral (pertrochanteric/intertrochanteric fractures).
Femoral neck fractures can be classified with Pauwel’s classification [7], which describes the horizontality of the fracture line or more commonly classified with Garden’s classification, which is based on the displacement of the fracture on an AP x-ray image [8] (Table 1) (Figure 2).
Table 1. Garden classification for femoral neck fractures.
| Type | Description |
|---|---|
| 1 | Incomplete fracture (or valgus impacted) |
| 2 | Complete fracture, not displaced |
| 3 | Complete fracture, partially displaced |
| 4 | Complete fracture, fully displaced |
And lastly, femoral head fractures are classified using the classic Pipkin’s classification [11]. Table 3. Figure 3.

Figure 3. Hip AP x-ray showing a trochanteric fracture (AO 31A2).
Table 3. Pipkin classification for femoral head fractures.
| Type | Description |
|---|---|
| Type 1 | Fracture is below the fovea/ligamentum. Does not involve the weight-bearing portion of the femoral head. |
| Type 2 | Fracture is above the fovea/ligamentum, and involves the weight-bearing portion of the femoral head. |
| Type 3 | Type 1 or 2 fracture associated with a femoral neck fracture. It has a high incidence of avascular necrosis. |
| Type 4 | Type 1 or 2 fracture associated with an acetabulum fracture, usually the posterior wall. |
Clinical Presentation of Hip Fractures
Patients with hip fractures will have pain in the hip or groin region, which can be referred to the medial side of the thigh or the knee. They are unable to walk or bear weight on the affected leg and sitting or logrolling elicits pain.
Classically, in the patient with a fractured hip, the affected leg will be shorter and externally rotated. There can be bruises or edema around the hip too.
Otherwise, when a femoral head fracture is associated with a hip dislocation, the affected hip and leg will be in slight flexion, adduction, and internal rotation. Testing of neurovascular structures is essential since hip dislocations are associated with sciatic nerve injuries in 10-20%[12].
There should be concern about other clinical symptoms and associated lesions in the elderly or polytrauma patients, especially head trauma and femoral shaft fractures, with are usually associated with hip fractures.
Imaging for Hip Fractures
The first and most valuable studies are Radiographs. The protocol should include at least a pelvic AP radiograph and a full-length ipsilateral femur x-ray to exclude associated femoral shaft fractures. Axial hip images or frog leg pelvis AP can be difficult to obtain since pain is usually severe, but cross-table lateral images can be achieved to address the displacement of the neck in the sagittal plane. Lastly, a traction-internal rotation pelvis AP image can show if the fracture is reducible and stable.
CT scan is helpful in determining displacement and degree of comminution in some patients but is mandatory in those patients with a femoral head fracture (intraarticular injury) or after a hip dislocation.
MRI imaging is useful in those cases where a stress fracture or occult fracture is suspected.
Initial Management of Hip Fractures
- ATLS protocol should be performed in patients with polytrauma (high energy injuries).
- Perform imaging protocol and confirm the diagnosis.
- After confirming the fracture, the patient should be admitted to the hospital (step-down unit) with absolute bed rest.
- Preoperative order set.
- Hip fracture is an independent risk factor for VTE. Start venous thromboembolism prophylaxis, possibly with Heparin.
- This injury should be considered an emergency; early operative treatment is fundamental. Evidence supports that hip fracture surgery within 48 hours of admission is associated with better outcomes. Even in elderly patients, early surgery within 24 hrs of admission is independently associated with fewer pulmonary complications, failure to extubate, reintubation, and shorter length of stay [13].
- In the case surgery can not be done in the 48 hours window, consider an anti-rotational short cast or boot or bone traction if the hip is severely displaced (moderate evidence is against the use of traction routinely).
Preoperative Medical Optimization for Patients with Hip Fractures
- Perform a risk assessment for any comorbidities and attempt to maximally optimize each comorbidity perioperatively.
- Orthogeriatics patients should be co-managed by medicine and surgery, and this has demonstrated a shorter time to surgery [14]. There is strong evidence for the use of an interdisciplinary care program in those patients with mild to moderate dementia to improve functional outcomes. Co-managed patients had lower mortality at 1 year [15].
- Consider regional analgesia to improve preoperative pain control (i.e epidural analgesia) when the patient arrives at the ER.
- Limited evidence supports not delaying hip fracture surgery for patients on aspirin and/or clopidogrel
- Limited evidence supports the preoperative assessment of serum levels of albumin and creatinine for risk assessment of hip fracture patients
- Tranexamic acid (TXA) is used at the beginning of the surgery and in the end to decrease perioperative bleeding and blood transfusion[16].
Operative Treatment for Hip Fractures
Femoral neck fractures
Several options exist for the treatment of femoral neck fractures, ranging from internal fixation to arthroplasty. AAOS recommends the use of internal fixation for stable, non-displaced fractures and arthroplasty for displaced fractures (in the elderly).
Fixation with cannulated screws is indicated in patients with nondisplaced transcervical fractures (Garden I) in physiologically young patients, or displaced transcervical fractures in young patients (Figure 4). The reduction must be anatomic, open reduction may be necessary. A sliding hip screw (SHS) is indicated for basicervical fractures or vertical lines in young patients. SHS is associated with lower reoperation rates compared to cannulated screws [17].

Figure 4. Cannulated screws on left hip for treatment of medial hip fracture.
Moderate evidence supports a benefit to total hip arthroplasty in properly selected patients with unstable (displaced) femoral neck fractures. The use of femoral cemented stems is recommended in femoral neck fractures. Hemiarthroplasty indications are controversial and should be considered in debilitated elderly patients or with metabolic bone disease. Outcomes of unipolar and bipolar hemiarthroplasty for unstable (displaced) femoral neck fractures are similar (Figure 5). Total hip arthroplasty is reserved for older active patients or patients with pre-existing hip osteoarthritis because outcomes include more predictable pain relief and better functional outcomes than hemiarthroplasty [18].
Femoral intertrochanteric fractures
Rich collateral circulation reduces the risk of non-union and avascular necrosis; therefore, internal fixation is the preferred treatment for lateral hip fractures. In stable intertrochanteric fractures, the use of either a sliding hip screw (SHS) or a cephalomedullary nail (CMN) is recommended. In unstable fractures and reverse obliquity fractures, a cephalomedullary nail (CMN) device is preferred (Figure 6). Arthroplasty indications are rare and include salvage for failed internal fixation, severely comminuted fractures, pre-existing severe hip arthritis, or severely osteoporotic bone that is unlikely to hold internal fixation.
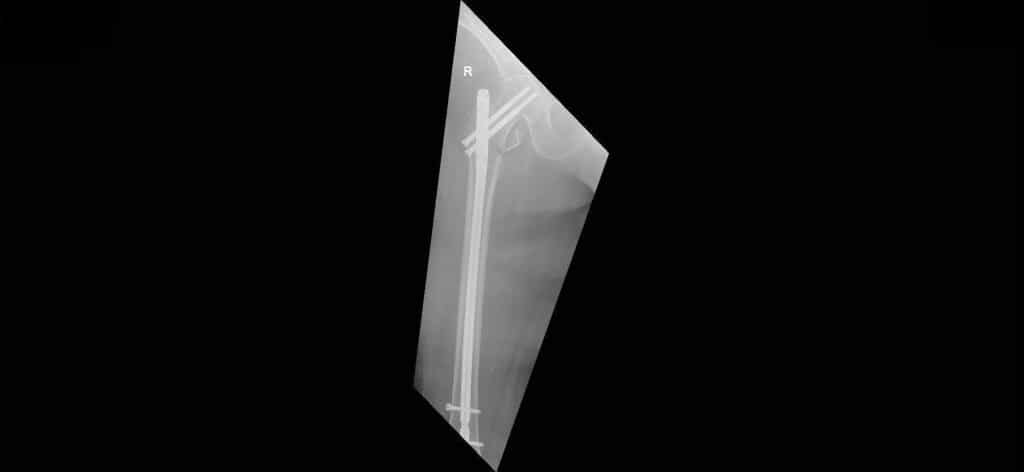
Figure 6. Full-length femoral AP radiograph showing a Cephalomedullary nail for an AO 31A2 fracture.
Complications of Hip Fractures
In femoral neck fractures incidence of osteonecrosis is 10-45% and is associated with a non-anatomical reduction and the initial displacement [19]. Non-union incidence is 5-30% and is associated with displaced fractures and varus malreduction. Dislocation after arthroplasty is common, too, with an incidence of 10% approximately. Internal fixation failure can be as high as 46% in the elderly population.
For intertrochanteric fractures, implant failure and cutout occur in 4-20% and are associated with older age, osteoporosis, quality of reduction, and screw positioning. Nonunion is much lower than in femoral neck fractures (<2%). 30% of patients will have hemoglobin lower than 8mg/dl requiring transfusion.
Prognosis of Hip Fractures
Mortality risk after the first year following fracture is 15-30%. More than 80% of those not treated operatively will die in the first year. Risk factors for high mortality include male gender, intertrochanteric fracture, operative delay of two days or more, older than 85 years, two or more pre-existing medical conditions, and ASA III or ASA IV preoperative score [20]. 41% of patients will maintain pre-injury ambulatory status. Loss of independence will be noted in 40% of patients, who will require assistive devices, 12% become household ambulators, and 8% will not ambulate anymore [21].
Disclosures:
The author does not report any conflict of interest.
Disclaimer:
This information is for educational purposes and is not intended to treat disease or supplant medical professional judgment. Physicians should follow local policy regarding the diagnosis and management of medical conditions.
See Also
Distal Radial Fractures in Adults
Bibliography
[7] Pauwels F. Der Schenkelhalsbruch. Gesammelte Abhandlungen Zur Funktionellen Anatomie Des Bewegungsapparates 1965:1–138. https://doi.org/10.1007/978-3-642-86841-2_1.

Follow us